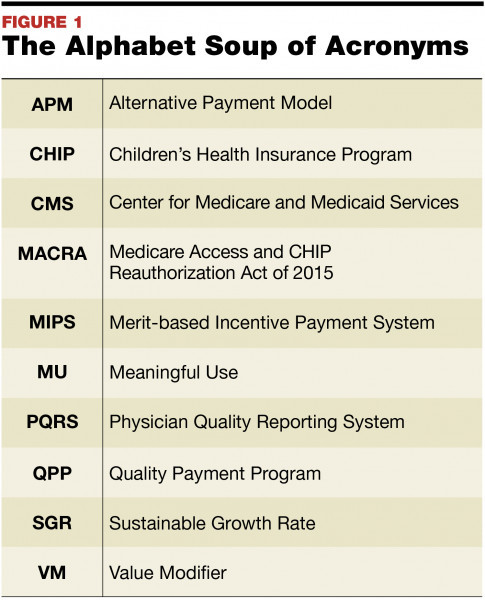
On september 21 2018 we selected 7 applicants to receive cooperative agreement awards through the medicare access and chip reauthorization act of 2015 macra funding.
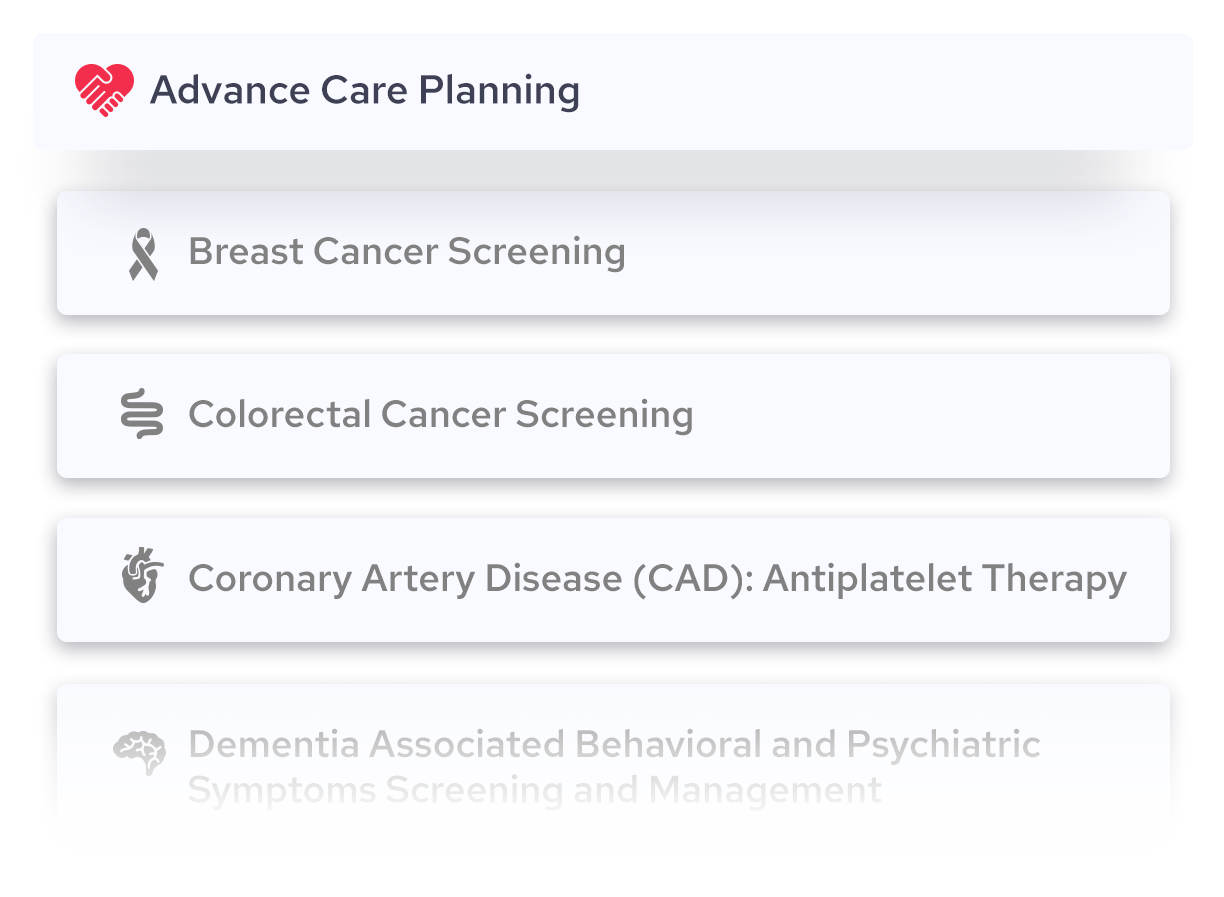
Macra quality measures list.
Qcdr measures or mips measures.
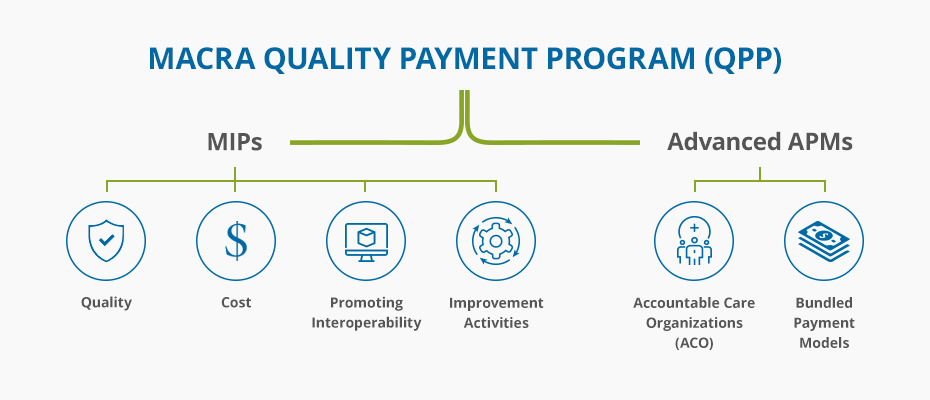
One way cms will pay providers under macra is through the merit based incentive payment systems mips.
2018 macra quality measures.
They have some very important.
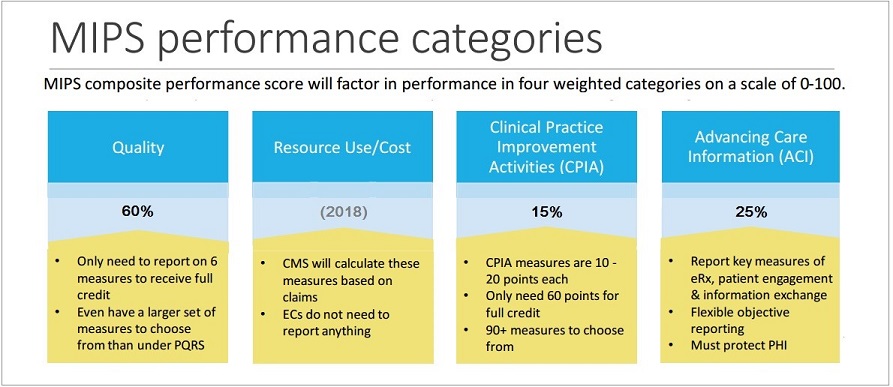
Under the merit based incentive payment system mips eligible clinicians continue to be paid on a fee for service basis and report cost and quality data following each performance year clinicians are evaluated on their performance relative to other clinicians in the country and receive a positive neutral or negative payment adjustment to their.
Quality measure bonus points can be earned in the following ways.
Types of macra quality measures.
Measure development for the quality payment program.
Macra codes are used by medical coders to report cost and quality measures.
Macra requires the plan to be posted on the cms gov website by may 1 2016.
The macra patient relationship codes are healthcare common procedure coding system hcpcs level ii modifier codes that enable clinicians to self identify their relationship with and responsibility for a patient at the time of furnishing an item or service.
Macra provides both a mandate and an opportunity for cms to leverage quality measure development as a key driver to further the aims of the cms quality strategy.
Qcdr measures or mips measures.
These measures come in 2 flavors.
Each provider must show their ability to meet goals in each of four sections.
These measures come in 2 flavors.
Cooperative agreement awardees.
Quality measures advancing care information resource use measures clinical practice improvement activities.
Medicare access and chip reauthorization act of 2015 macra funding opportunity.
Submission of 2 or more outcome or high priority quality measures bonus will not be awarded for the first outcome or high priority quality measure submission using end to end electronic reporting.
Abg qcdr shared qcdr and mips measures defined.
Quality measures account for 75 of your composite performance score cps and you can only report a maximum of 6 measures.
Mips merit based incentive payment system.
You can achieve success in macra quality measures using certified health it under the centers for medicare medicaid services cms merit based incentive payment system mips program quality is one of the four measurement categories that impact your overall score and it s worth the most points toward your final score 60 points.
Commenters informed the creation of this final cms quality measure development plan mdp.
They have some very important.